Gender-affirming care for minors under fire in sweeping US report
Federal investigators found that thousands of children received irreversible medical interventions despite weak evidence, ethical lapses, and inadequate safeguards.
Paediatric gender dysphoria has rapidly emerged as one of the most divisive and urgent issues in medicine today. In the past decade, the number of children and adolescents identifying as transgender or nonbinary has soared.
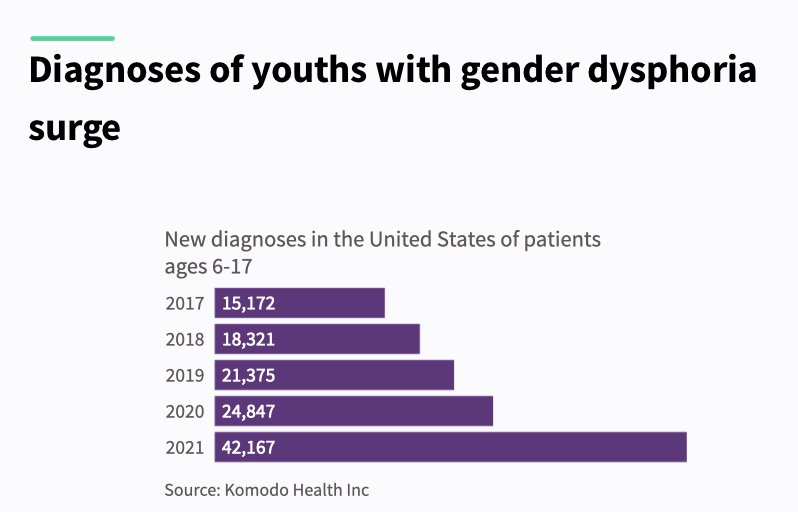
In the US alone, diagnoses among youth aged 6 to 17 nearly tripled—from around 15,000 in 2017 to over 42,000 by 2021—signalling a seismic shift not only in culture but in clinical practice.
Children diagnosed with gender dysphoria—a condition defined by distress related to one’s biological sex or associated gender roles—are increasingly being offered powerful medical interventions.
These include puberty blockers, cross-sex hormones, and, in some cases, irreversible surgeries such as mastectomy, vaginoplasty, or phalloplasty.
An umbrella review from the US Department of Health and Human Services (HHS) states that “thousands of American children and adolescents have received these interventions,” despite a lack of solid scientific footing.
While advocates often claim the treatments are “medically necessary” and “lifesaving” the report concludes “the overall quality of evidence concerning the effects of any intervention on psychological outcomes, quality of life, regret, or long-term health, is very low.”
It also cautions that evidence of harm is sparse—not necessarily because harms are rare, but due to limited long-term data, weak tracking, and publication bias.
This 409-page report delivers a scathing review of the assumptions, ethics, and clinical practices driving gender-affirming care in the US.
An inversion of medical ethics
At the heart of the HHS critique is a reversal of medical norms.
“In many areas of medicine, treatments are first established as safe and effective in adults before being extended to paediatric populations,” the report explains. “In this case, however, the opposite occurred.”
Despite inconclusive outcomes in adults, these interventions were rolled out for children—without rigorous data, and with little regard for long-term, often irreversible consequences.
These include infertility, sexual dysfunction, impaired bone development, elevated cardiovascular risk, and psychiatric complications.
“The physical consequences are often irreversible,” the report warns.
Puberty blockers, frequently marketed as a reversible ‘pause,’ actually interrupt bone mineralisation at a critical growth stage—raising the risk of stunted skeletal growth and early-onset osteoporosis.
When followed by cross-sex hormones, as is common, the harms multiply. Known risks include metabolic disruption, blood clots, sterility, and permanent loss of sexual function.
Yet many clinics operate under a “child-led care” model, where a minor’s self-declared “embodiment goals” dictate treatment.
The report notes that some leading clinics conduct assessments “in a single session lasting two hours,” often with no robust psychological evaluation.
Consent and capacity
This raises a critical question: are children capable of consenting to life-altering medical interventions?
According to the HHS, informed consent means more than simple agreement—it requires a deep understanding of risks, alternatives, and long-term impact.
And by definition, children lack full legal and developmental capacity for medical decision-making.
“When medical interventions pose unnecessary, disproportionate risks of harm, healthcare providers should refuse to offer them even when they are preferred, requested, or demanded by patients,” the report states.
Supportive parents cannot shield clinicians from ethical responsibility. Many children who present for transition also have autism, trauma histories, depression, or anxiety—all of which can impair decision-making.
Yet clinicians frequently misread a child’s desire to transition as evidence of capacity.
The report warns that the current affirmation model “undermines the possibility of genuinely informed consent” and that the “true rate of regret is not known.”
This becomes especially urgent when the outcomes—sterility, bone loss, and sexual dysfunction—are permanent. Can a 13-year-old grasp what it means to forgo biological parenthood?
As the report suggests, the system has failed to distinguish between a young person’s wish to transition and their developmental ability to understand what that means long term.
A moral failure
The problem is not only medical—it’s moral.
The HHS accuses the medical establishment of abandoning its core duty: to protect vulnerable patients. Ideology and activism, it argues, have taken precedence over evidence and caution.
“The evidence for benefit of paediatric medical transition is very uncertain, while the evidence for harm is less uncertain,” it states.
Among the most disturbing trends highlighted in the report is the sidelining of mental health support.
Research suggests that most cases of paediatric gender dysphoria resolve without intervention. Yet clinicians continue to proceed with irreversible treatments.
“Medical professionals have no way to know which patients may continue to experience gender dysphoria and which will come to terms with their bodies,” the report explains.
The illusion of consensus
The report also takes aim at the idea that gender-affirming care enjoys universal professional backing. It reveals that many official endorsements come from small, ideologically driven committees within larger organisations.
“There is evidence that some medical and mental health associations have suppressed dissent and stifled debate about this issue among their members,” it warns.
Several whistleblowers have spoken out—often at considerable personal risk.
Jamie Reed, a former case manager at the Washington University Transgender Center, alleged that children were being rushed into medical transition without adequate psychological screening. Her testimony led to a state investigation and Senate hearing.
Clinical psychologist Erica Anderson, a transgender woman and former president of the US Professional Association for Transgender Health, has repeatedly raised concerns about the haste with which children are put on medical pathways.
Dr Eithan Haim, a surgeon in Texas, is now facing prosecution after revealing details about paediatric gender surgeries at a children’s hospital.
Rather than sparking debate, these whistleblowers have faced vilification, career damage, and in some cases legal consequences. The HHS suggests this culture of fear has stifled the scientific inquiry necessary for sound medicine.
Psychotherapy as an alternative
Instead of defaulting to hormones or surgery, the report urges a return to psychotherapy. Gender-related distress, it notes, often overlaps with broader psychological challenges that can be addressed non-invasively.
“There is no evidence that pediatric medical transition reduces the incidence of suicide, which remains, fortunately, very low,” the report finds.
Psychotherapy carries no documented harms and offers space for resolution and support. The HHS calls for greater investment in “psychotherapeutic management” as a safer and more ethical approach.
Restoring scientific integrity
Commissioned under President Trump’s Executive Order Defending Children’s Innocence by Ending Ideological Medical Interventions, the report responds to growing alarm over the medicalisation of minors.
Trump’s Executive Order directed federal agencies to evaluate practices to help “minors with gender dysphoria, rapid-onset gender dysphoria, or other identity-based confusion, or who otherwise seek chemical or surgical mutilation.”
It explicitly criticised “junk science” promoted by groups such as the World Professional Association for Transgender Health (WPATH), calling for a return to evidence-based standards and scientific discipline.
Rather than imposing new mandates, the HHS report focuses on delivering “the most accurate and current information available” to clinicians, families, and policymakers—urging caution and restraint.
“Our duty is to protect our nation’s children—not expose them to unproven and irreversible medical interventions,” said NIH Director Dr Jay Bhattacharya. “We must follow the gold standard of science, not activist agendas.”
Reform already underway
The HHS report lands amid a wave of legal reforms.
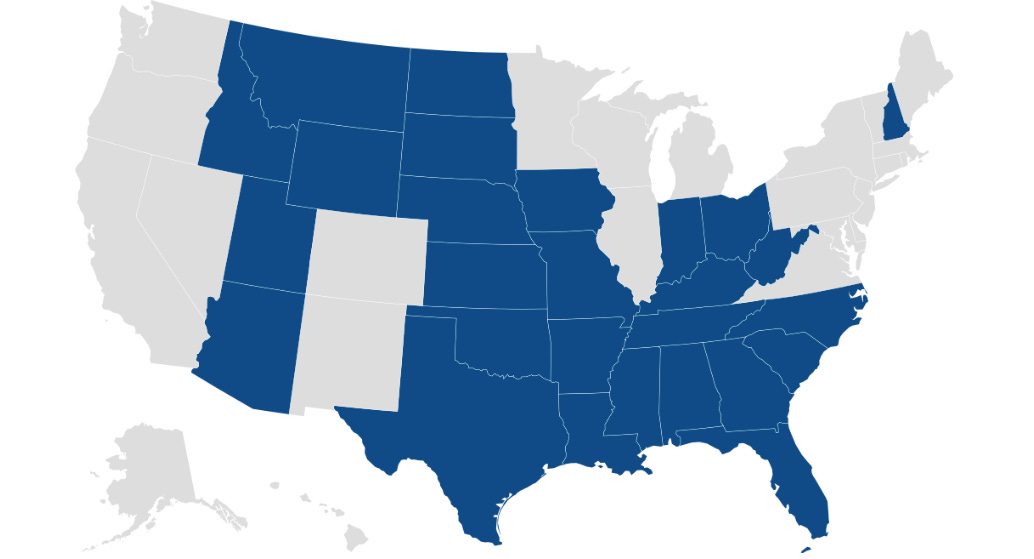
As of this year, 27 states have passed laws restricting or banning gender-affirming care for minors. These range from full bans on hormones and surgery to tighter consent requirements.
Nineteen of those laws were passed in 2023 alone, according to the Kaiser Family Foundation.
Though many face court challenges, the trend reflects mounting public concern over the medicalisation of gender-distressed youth. The HHS findings are expected to accelerate further scrutiny and legislative action.
Global shifts
The HHS review is part of a broader international movement to re-examine paediatric gender medicine.
In 2024, the UK’s Cass Review, led by paediatrician Dr Hilary Cass, delivered a landmark critique of NHS gender services. Cass concluded that the model had been adopted prematurely “based on a single Dutch study,” and lacked sufficient evidence.
In response, the UK banned the routine use of puberty blockers and began closing the Tavistock gender clinic, replacing it with regional centres focused on holistic mental health care.
In Australia, the Queensland government took similar steps earlier this year, pausing all prescriptions of puberty blockers and cross-sex hormones for minors pending further review.
The move followed the suspension of Dr Jillian Spencer, a senior psychiatrist, from her clinical duties at Queensland Children’s Hospital after she raised concerns about the gender care protocols being used.
Her case has since become a focal point in Australia’s national debate on youth gender medicine.
A reckoning
The HHS report is more than a policy review—it is a warning.
It reveals that thousands of children—many struggling with underlying psychological issues—have been placed on a path of irreversible medicalisation without the basic safeguards expected in any other area of healthcare.
The report concludes that gender medicine has been practised backwards - treatments were introduced first, and only later did the search for evidence begin.
It calls for a course correction—one that puts evidence before ideology, and ethics above political expediency.
Whether institutions will act on its findings remains to be seen. But for families searching for answers, the report may finally provide the long-overdue clarity that has been obscured by years of activism and politics.








Gender dysphoria in many cases is not a primary condition, but rather a secondary or symptomatic manifestation of broader psychological or neurodevelopmental disturbances such as autism spectrum traits, interoceptive deficits, or identity instability. The vast majority of individuals with "gender dysphoria" ultimately desist, particularly during adolescence. What they need is support, not aggresive medicalization.
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.632784/full
To aggressively medicalize these individuals without comprehensive assessment and truly informed consent constitutes a clinical and ethical aberration. There is a global push to obscure the true nature of this diagnosis and suppress the full picture to get a true informed consent. Many psychologists says they "affirm", but the role of a psychologist is not to affirm, but to exercise clinical discernment, exploring the full complexity of the individual’s presentation to guide clinical and ethically sound decisions. They only "affirm" what they wish, or are instructed, to see. A significant amount of people is aware about bias in medicine, but psychology… One day, we’ll have to talk about what’s really going on psychology faculties.
I've studied extensively about the dark side of medicine, but rarely have I encountered something as maliciously intended as this. To me, the real problem is that law no longer functions as a safeguard. It’s dead in essence, if not in form. Harmed individuals are no longer protected. Freedom of expression is no longer defended. Those who lie and cause harm thrive.
Thank you, Maryanne. I think Dr Jillian Spencer is a hero for speaking out.
I'm a clinical psychologist (not in general private practice anymore), who has long held concerns over how ideology infects health policies and guidelines. It seems to me that many professional bodies are not courageous and critical enough when it comes to separating ideology from evidence-based health care. That 'gender affirming care' infiltrated hospital and health care systems in Australia, with minors allegedly 'consenting' to irreversible medical interventions on the basis of gender dysphoria, remains deeply shocking to me. I don't believe these doctors are intending to cause harm, but it appears their rush to display good intentions / 'kindness' / 'equality' etc has overrun basic ethical decision-making. Medicine and psychology must not prioritise feelings over facts.